NC State and UNC-Chapel Hill researchers working on breakthrough cardiac treatment
How do you cure a broken heart?
If you’re researcher Ke Cheng, hopefully one day soon, it will be with a simple injection.
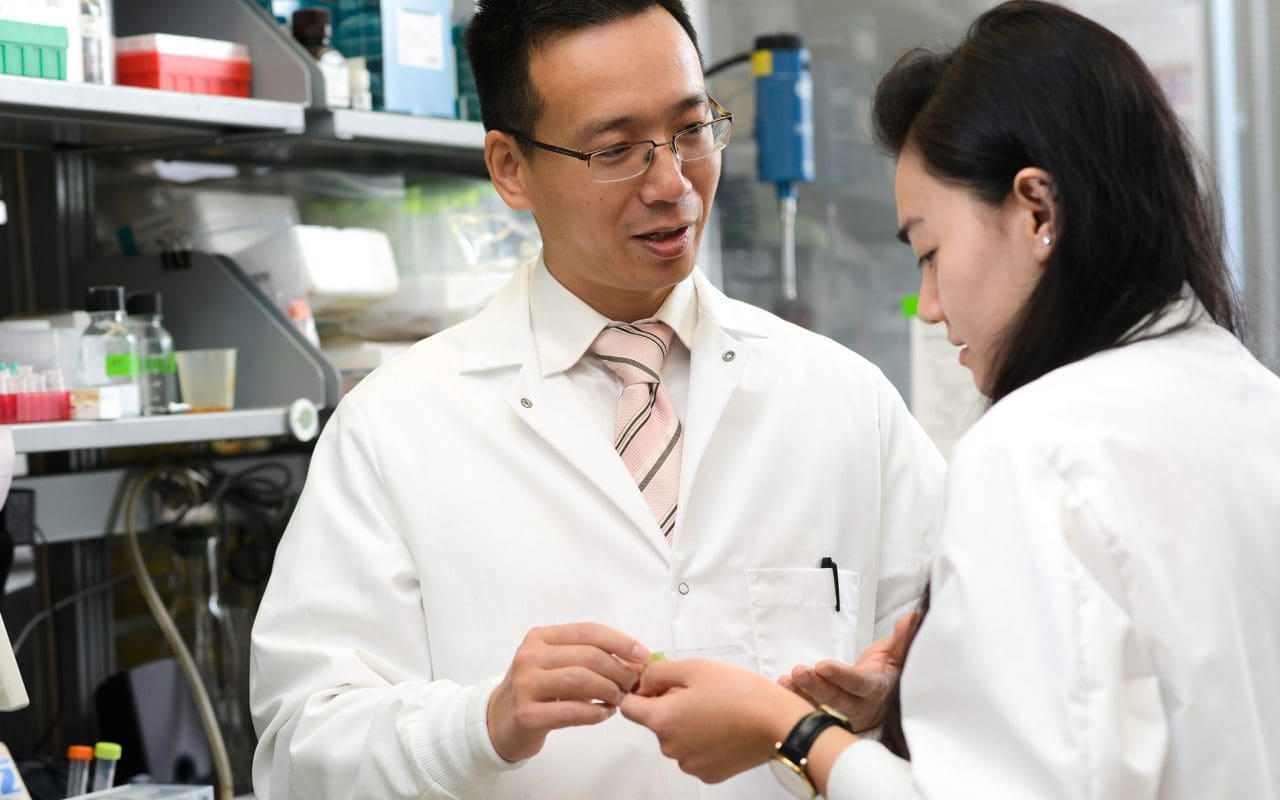
Cheng, an associate professor in the college of veterinary medicine at North Carolina State University and biomedical engineering department (a joint program between NC State and the University of North Carolina at Chapel Hill), isn’t out to cure the metaphorical broken heart, of course. Rather, he and his research team are devising a method using synthetic stem cells that could one day fix many heart ailments through non-surgical means. Cheng and his research partner, Dr. Thomas Caranasos of the University of North Carolina School of Medicine, have created a way to harvest the healing factors secreted by heart stem cells and encapsulate them synthetically. They recently patented the process and published their findings.
Cheng has worked on stem cell therapy for years, going back to his days at Cedars-Sinai Medical Center in Los Angeles. It was there he first learned the process of harvesting cells from a patient that could be used to treat that patient’s ailment. But using stem cells in lieu of a traditional medicine does have its limitations, Cheng said.
It’s important to note that the cells Cheng uses are adult stem cells harvested from patients and donors, and are not taken from embryos.
“The stem cells aren’t a pill – they are live organisms,” he said. “A huge limitation is how to store them and how to maintain stability. A limitation of stem cell therapy is that oftentimes, we have to prepare them fresh. It’s not like taking a powder and making it a pill, then storing on a shelf for a couple of years. With stem cells, you take the biopsy, grow the cells in the lab, then take it back to the patient.”
Cheng was left with a puzzle – how to best utilize the healing power of the stem cells but maintain them in such a way that they can last over a period of time. It can take a month to grow the necessary number of stem cells to treat a patient, and there’s always a risk the cells can be contaminated, so the process is far from simple.
“Off-the-shelf is important for any medicine, because a patient can come to you at any time, and you need to be able to offer him the medicine off the shelf as soon as possible,” he said. “Stem cell therapy doesn’t have that.”
Another major obstacle is the lack of control once the patient is injected with stem cells. If the stem cells reproduce too much inside the body, it could likely lead to the growth of tumors. Still, according to Cheng, the benefits of stem cell therapy are too great to just give up on.
“I see stem cells as little pharmacies,” he said. “They secrete a great many things that are beneficial to the body. These factors can promote repair in the heart, lungs and liver – all kinds of things. So, instead of using the cells themselves, we want to use the factors they secrete – instead of using the cow, we harvest the milk instead.”
But harvesting those proteins isn’t enough. It’s not as simple as creating a liquid medicine that can be injected into the patient. Rather, the medicine needs to be delivered in a time-release fashion.
“We encapsulate all these factors into a biodegradable polymer micro-particle,” he said. “It’s exactly the same size as a cell, about 20 microns. Once they degrade, they release the factors that we package in them. They gradually release the stem cell release factors that we can inject into the heart.”
The micro-particles, containing the stem cell-secreted factors, are then encased in stem cell membranes, so that the micro-particles can link up with the injured cells to repair them. The completed particle is called a cell-mimicking micro-particle, or a synthetic stem cell by its function.
The beauty of synthetic stem cells is that they can be frozen or turned into a powder, giving them a long shelf life. In addition, the original stem cells don’t necessarily have to come from the patient – they can come from any donor cell that proves viable. In addition, they can be mass-produced and stored relatively cheaply.
The funding for Cheng and Caranasos’ research came from a grant from the University of North Carolina’s Research Opportunities Initiative. Cheng said his team is seeking more grant funding for testing on more comprehensive animal models. If that animal testing is successful, the team will seek for FDA permission to start human trials, perhaps within the next five years.
“The original intention of the UNC Research Opportunities Initiative was to fund research projects that could truly shift current paradigms in science and medicine,” said Erin Hopper, Research Director at UNC General Administration. “Dr. Cheng’s and Dr. Caranasos’ impressive research outcomes exemplify the fundamental goals of this grant program, and we look forward to watching their work continue to develop.”
Other researchers are already picking up on Caranasos and Cheng’s work.
“Already, people have contacted us,” Cheng said. “They are interested in neural stem cells for brain disease and spinal cord injuries. This technology, I call it ‘platform technology,’ which means it is universal and can be generalized to other organs as long as you can harvest the factors and encapsulate the membrane, you can make artificial t-cells, artificial stem cells, even artificial cancer cells to use as a vaccine. So it has other implications as well.”
Cheng got his undergraduate degree in his native China and earned his doctorate at the University of Georgia. While doing research at Cedars-Sinai and UCLA, he heard about the Chancellor’s Faculty Excellence Program at NC State.
“I thought it would be a nice opportunity to expand my research,” he said. “Also, NC State has a strong engineering background and the students are smart. What I wanted to do is join all the forces in training and experience that I have ever received.”